About Us
On This Page:
The Office of Johns Hopkins Physicians (OJHP) was established to coordinate the activities of the Clinical Practice Association, Johns Hopkins Community Physicians and all physicians now part of or joining Johns Hopkins Medicine (JHM), regardless of entity or location. OJHP will ensure that the necessary resources and coordination are in place to allow all physicians to support Johns Hopkins Medicine and its mission.
To ensure that OJHP has the broadest possible perspective on and influence across Johns Hopkins, the new office works with other key groups and people within JHM. For example, the new Johns Hopkins Health System senior vice president for the Community Division, the presidents of the member hospitals and the vice presidents for medical affairs at each of the member hospitals will coordinate physician activities in their respective areas with the OJHP.
OJHP develops overall guidelines and parameters to assist in the development of new physician offices, physician activities and physician engagement throughout JHM. In addition, it works in partnership with Johns Hopkins Health Plans as JHM responds to health care reform and moves forward with the development of the new Johns Hopkins care delivery model.
Mission and Vision
OJHP is responsible for assessing the current state of Johns Hopkins physicians, examining unmet physician needs throughout the JHM family, developing strategies for meeting current and unmet needs for Johns Hopkins physician services and ensuring, in all such endeavors, that Johns Hopkins physicians are supported in a way that fosters Johns Hopkins’ tripartite mission. The vision is to create clinical integration among all physicians within JHM, leading to a patient-centered care delivery system anchored in research and education.
What We Do
OJHP coordinates the activities not only of the Clinical Practice Association (CPA) and Johns Hopkins Community Physicians (JHCP), but also the activities of all physicians now part of or joining the JHM family, regardless of entity or location within JHM, including physicians who are employed by JHCP, employed by the Johns Hopkins community hospitals as hospitalists and employed through health system affiliates and those with whom affiliates have aligned. The office ensures that the necessary planning committees are put in place, that resources are made available and that coordination takes place to support Johns Hopkins physicians and in turn JHM.
The office oversees the engagement of Johns Hopkins physicians. The Clinical Physician Recruitment Guiding Principles build a process for the engagement of all new community specialists and hospitalists throughout JHM. Through this process, the Johns Hopkins University School of Medicine directors will be involved in the recruitment and quality oversight of these Johns Hopkins physicians, while still meeting the clinical needs of our community affiliates.
In addition, the office coordinates administrative services to support Johns Hopkins physician practices wherever they are located. This provider support function will use existing JHM resources to the extent possible, but will advocate for additional resources as needed for this function.
Our Leadership
Conway, Sarah Johnson, M.D.
Chief Medical Officer, Johns Hopkins Clinical Alliance
Assistant Professor of Medicine
Helicke, Melissa, M.B.A., M.H.A.
Vice President and COO, Office of Johns Hopkins Physicians
Executive Director, Clinical Practice Association
Vice President, Johns Hopkins Medicine

Kravet, Steven Jay, M.D., M.B.A.
President, Johns Hopkins Community Physicians
Associate Professor of Medicine

Key Initiatives by Name
Jon Efron, M.D.
- Clinical Excellence Awards
- Managed Care Contracting
Melissa Helicke
- Ambulatory Operations
- Ambulatory Strategy
- Access Services
- Executive Preventive Health
- Professional-Fee Billing
- Physician Alignment and Contracting
Lisa Ishii, M.D.
- Clinical Integration
- Clinical Pathways and Protocols
- Ambulatory Surgery Center Coordinating Council
Sarah Johnson Conway, M.D.
- FQHC
- Total Cost of Care
- NCR Provider Alignment
Peter Greene, M.D.
- Epic and Health IT Strategy and Coordination
- Data Governance and Analytics
Peter Hill, M.D.
- Provider Credentialing
Scott Berkowitz, M.D.
- Accountable Care
Stephen Sisson, M.D.
- Johns Hopkins Medicine Ambulatory Operations, Quality, Safety and Service
- Johns Hopkins Medical Management Corporation
Steve Kravet, M.D.
- Primary Care Strategy
- Ambulatory Quality and Safety
- Ambulatory Patient Satisfaction
- Maryland PCP
Brian Hasselfeld, M.D.
- Digital Health and Innovation
OJHP Scope of Practice
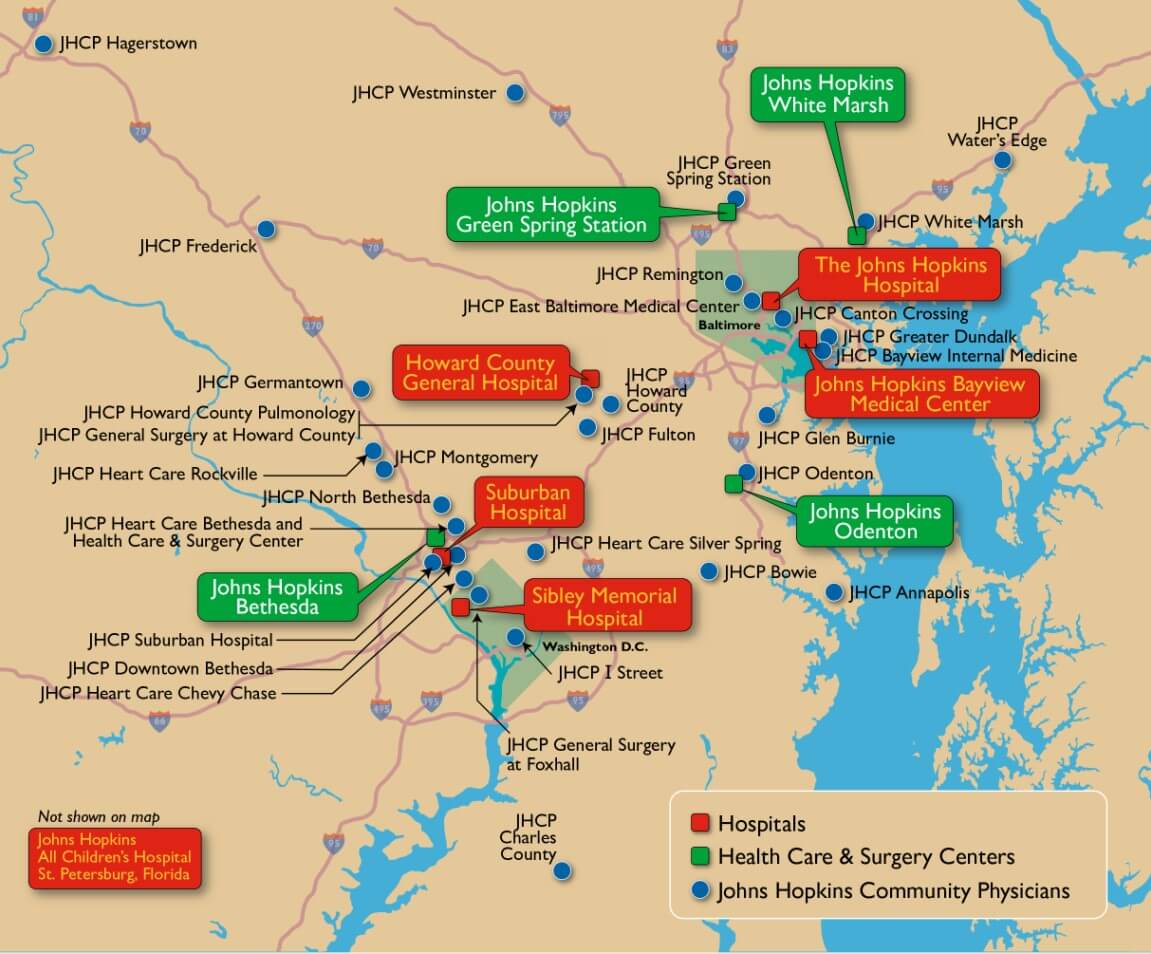
The Office of Johns Hopkins Physicians continues to expand and grow in the number of faculty members, outpatient clinic locations, and outpatient clinic visits. Currently, OJHP is comprised of over 2,100 physicians. Annual ambulatory outpatient visits currently total 2.8 Million. Ambulatory services are currently provided on 52 campuses in four states (MD, PA, VA, FL) and DC.
Additionally, our clinical specialties rank among the highest in the nation. Among the top specialty rankings for adult patients are Rheumatology (ranked #1), Neurology and Neurosurgery (ranked #2), and Ear, Nose & Throat, Gastroenterology & GI Surgery, and Ophthalmology (ranked #3) nationwide.
This year, seven of Johns Hopkins Children's Center's specialties were ranked among the top 10 nationally, with two appearing in the top five. Please join us in congratulating the following divisions on their rankings:
- #4: Neonatology
- #5: Neurology & Neurosurgery
- #6: Cancer
- #7: Urology
- #9: Gastroenterology & GI Surgery
- #10: Orthopedics
- #10: Pulmonology
- #11: Nephrology
- #12: Diabetes & Endocrinology
- #34: Cardiology & Heart Surgery
We are also pleased to report that Johns Hopkins All Children's Hospital in St. Petersburg, Florida, ranked nationally in three specialties: Neurology & Neurosurgery, Cardiology & Heart Surgery and Orthopedics. For a complete list of the Best Children's Hospitals, please visit the U.S. News & World Report website.
