Radiology Exam: Functional MRI
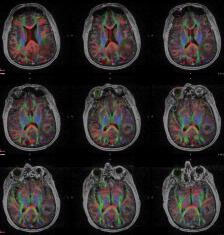 DTI axial fMRI
DTI axial fMRI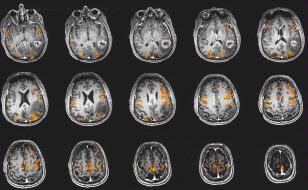 BOLD fMRI
BOLD fMRIClinical functional MRI involves both blood oxygen level dependent (BOLD) functional magnetic resonance imaging (fMRI) and diffusion tensor imaging (DTI). These are usually performed together since they provide complementary information that can be used by neurosurgeons to evaluate risks associated with planned surgical intervention, plan their surgical approach, and assess the need for and possibly guide their intraoperative mapping procedure. fMRI and DTI are usually requested by neurosurgeons for presurgical planning purposes in patients with brain tumors or other structural brain lesions who are being evaluated for possible surgical intervention. The main reason for performing these exams is to determine proximity of important functional cortical regions (or “eloquent cortex”) to known brain structural lesions, with determination of hemispheric language dominance as a secondary consideration.
fMRI is used to evaluate subtle regional blood flow changes in brain cortex that occur during patient performance of specific tasks while inside the bore of a high-field MRI scanner (generally, at a field strength of 3 Tesla). Such tasks usually last anywhere from three to six minutes each and may involve repetitive movement of a part of the body, such as the hand, tongue, lip or foot, or may involve performance of specific language or visual tasks. All of these tasks are explained in detail to patients before they enter the scanner, and patients have the opportunity to practice these as well during a pre-scan training session to ensure that they can perform all tasks well. The patient’s performance of these tasks in the training session, as well as other factors, such as the patient’s neurologic deficits and brain lesion location on anatomic imaging, determine which tasks the neuroradiologist prescribes for the examination. After detailed statistical analysis of the raw images obtained from the scan (usually a few hours after completion of the scan), “activation maps” are generated that are based on analysis of results of each task (“paradigm”), as well as strict image quality control analysis. These maps are then reviewed directly with the referring neurosurgeon to assist him/her in planning the surgery or devising an alternative treatment plan. DTI is used to map eloquent white matter by delineating the relationships of important white matter tracts to known structural brain lesions that are potentially resectable. These white matter tracts are as important as overlying cortex because they serve as connections between different functional brain cortical regions. The combination of both BOLD fMRI and DTI provide a more comprehensive functional road map for the neurosurgeon than either modality alone.
While many other factors are considered in the surgical decision-making process, including results of and candidacy for intraoperative awake or asleep mapping, structural (including vascular) anatomy, lesion characterization and the patient’s overall preoperative neurological and medical status, the information that we can provide through presurgical functional mapping can contribute to a more complete picture of the risks and benefits of surgical intervention and can provide valuable information that the surgeon can use to plan his operation. For more information, please see the American Society of Functional Neuroradiology website at www.asfnr.org.
