-
Amir Hekmat Hamrahian, M.D.
- Medical Director of the Comprehensive Adrenal Center
- Associate Professor of Medicine
-
Lilah Fran Morris-Wiseman, M.D.

- Chief, Johns Hopkins Division of Endocrine Surgery
- Associate Professor of Surgery
- Associate Professor of Oncology
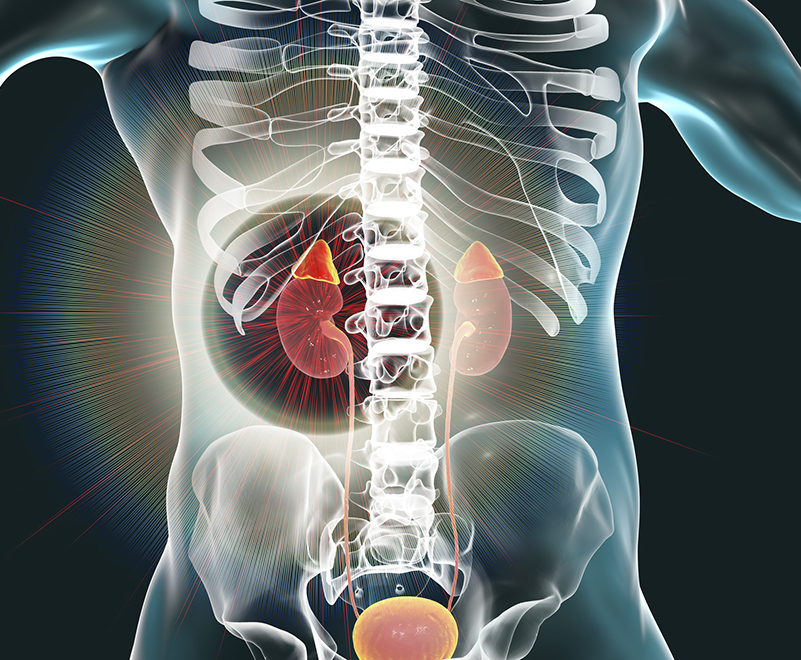
Johns Hopkins Comprehensive Adrenal Center
Adrenal disorders are complex and require a healthcare provider that has expertise with these conditions for the best outcomes. At the Johns Hopkins Comprehensive Adrenal Center, our team has that expertise.
The Johns Hopkins Comprehensive Adrenal Center is a multidisciplinary center consisting of a team of endocrinologists, surgeons, obstetricians, genetic counselors, radiologists, pathologists, nurse practitioners and nurses.
Conditions We Treat
The Johns Hopkins Comprehensive Adrenal Center treats the following conditions and performs the following procedures for diagnosis and treatment.
Conditions We Treat
- Adrenal myelolipoma
- Adrenal virilizing and feminizing tumors
- Adrenocortical carcinoma
- Congenital adrenal hyperplasia
- Cushing syndrome
Procedures We Offer
Why Choose Johns Hopkins for Adrenal Care?
The Johns Hopkins Comprehensive Adrenal Center is a unique center involving world-renowned specialists in every aspect of adrenal care. Our experts are leading adrenal research informing the most advanced diagnosis, treatment and care available.
Multidisciplinary Treatment
Our multidisciplinary team provides specialized diagnosis and treatment for each patient with a suspected or confirmed adrenal disorder.

Accurate Diagnosis
The Johns Hopkins Comprehensive Adrenal Center offers sophisticated dynamic endocrine testing to diagnose, treat and manage adrenal conditions.

Specialized Care
If diagnosed with an adrenal tumor, your care will be reviewed by our tumor review board harnessing the collective power of tumor care experts.
World-renowned Specialists
Our experts are leaders in adrenal care providing paramount education to care providers around the world.
Endocrine Dynamic Testing
Our center provides advanced testing to accurately diagnose adrenal disorders.
-
What is it?
Adrenocorticotropic hormone (ACTH) is made in the pituitary gland. The pituitary gland is a pea-sized gland at the base of the brain. One function of the pituitary gland is to control the amount of a hormone called cortisol. Cortisol is made in the adrenal glands which are above the kidneys. It is important for regulating many body functions such as:- Response to stress
- Ability to fight infection
- Maintenance of blood pressure
- Regulation of blood sugar
The test is done to diagnose ACTH or cortisol deficiency, a condition named adrenal insufficiency.
Preparation:
Certain medicines may be held, but there are no other restrictions. It can be done any time of day, and you do not have to fast.
Length of test:
The visit lasts approximately 90 minutes and includes registration, placing the IV, and doing the test.
Procedure:
An IV is placed in a vein in your arm to prevent multiple needle sticks. After the IV is placed, the needle is removed and a small, flexible catheter remains. Blood is drawn to see your levels before the cosyntropin is given. Cosyntropin is a man-made form of ACTH. It is given as an injection in the muscle of your upper arm. Blood levels are then drawn 30 minutes after the injection, and again at 60 minutes.
Possible side-effects:
There is a small chance you may feel flushed or nauseous after getting the cosyntropin.
Other side-effects are related to the IV and include:- Bleeding from the IV insertion site
- Bruising
- Lightheadedness
- Infection- rare as sterile technique is used
- Hematoma-blood under the skin
- Multiple punctures to locate veins
Results:
Results are available in a week. Please contact your doctor if you are not called about the result. -
Why is it done?
The adrenocorticotropic hormone (ACTH) stimulation test is done to diagnose an enzyme deficiency in the adrenal gland. In women, this may be associated with excess hair, acne, and menstrual problems. In men, problems fathering children may occur, but this is rare.Preparation:
The endocrine nurse will review your medicines, vitamins, and supplements with you. Some drugs can affect the results and need to be stopped before the test. Patients taking hydrocortisone or prednisone for adrenal insufficiency need to hold the medicine for 24 hours before the test (last dose in the morning the day before the test). The test can be done any time of day, and you do not have to fast.Length of test:
The test takes about 90 minutes, and includes registration, placing an IV, testing, and discharge.Procedure:
An IV is placed in a vein in your arm or hand. After the IV is placed, the needle is removed, and a small, flexible catheter remains. An IV is used, so you don’t have to get multiple needle sticks. Blood is drawn before getting Cosyntropin, a man-made form of ACTH. It is given as an injection in the muscle of your upper arm. Blood levels are drawn 60 minutes after the injection. The IV is removed and you are free to go home.Possible side-effects:
There is a small chance you may feel flushed or nauseous after getting the cosyntropin.
Other side-effects are related to the IV and include:- Bleeding from the IV insertion site
- Bruising
- Lightheadedness
- Infection- rare as sterile technique is used
- Hematoma-blood under the skin
- Multiple punctures to locate veins
Results:
Results are available in a week. Please contact your doctor if you are not called about the result. -
Why is it done?
The Captopril Challenge test is done to diagnose primary aldosteronism or hyperaldosteronism, a condition in which the body makes too much of the hormone, aldosterone. It leads to high blood pressure and may be associated with low potassium levels in some patients. In patients with hyperaldosteronism after taking a blood pressure medication called captopril, the aldosterone level does not decrease to the same level as in patients without the disease.
Preparation:
The endocrine nurse will review all your medicines, vitamins, and supplements with you. Some medicines for blood pressure, your heart, water pills (diuretics), and non-steroidal anti-inflammatory drugs for pain can affect the test and may need to be stopped.
You need to have your blood checked for a potassium level one week before the test. If your potassium is low, potassium pills will be given. Another blood draw may be needed to make sure the level is normal.
We ask that you eat a light snack if you need to take any medications with food. Otherwise, come to the clinic fasting. You may drink water as needed.
How long is the test?
The test takes 3 ½-4 hours, and includes registration, placing an IV, doing the test, and discharge. Feel free to bring music or something to read. Internet access is available.
Procedure:
The test is done while you are seated. After sitting for an hour, an IV is placed in a vein in your arm or hand. After the IV is placed, the needle is removed, and a small, flexible catheter remains. An IV is used so you don’t have to get multiple needle sticks. Blood samples are obtained and then you are given a blood pressure pill called Captopril. Blood samples are drawn one and two hours after taking the medicine. The endocrine nurse will check your blood pressure during the testing.
The IV is removed, and you are free to go home.
Possible side-effects:
Lightheadedness or dizziness
Other side-effects are related to the IV and include:- Bleeding from the IV insertion site
- Bruising
- Lightheadedness
- Infection- rare as sterile technique is used
- Hematoma-blood under the skin
- Multiple punctures to locate veins
Results:
Results are available in a week. Please contact your doctor if you are not called about the result. -
Why is it done?
The Clonidine Suppression test is performed to see if there is a rare adrenal tumor (called a pheochromocytoma) or an extra adrenal tumor (called a paraganglioma). Both conditions can be associated with a number of symptoms including significant elevation in blood pressure, headache, excess sweating, chest pain and rapid heartbeat.
Preparation:
The endocrine nurse will review all your medicines, vitamins, and supplements with you. Some medicines such as anti-hypertensive drugs and some of the pills used to treat anxiety/depression can affect your blood result and may need to be stopped before the test.
You must fast for 10 hours before, as well as during the test. Water is permitted.
Avoid exercise or smoking the morning of the test.
Please do not take your medicines the morning of the test unless you have discussed them in advance with your physician performing the test. Patients are generally advised to hold their anti-hypertensive medications the morning of the test. You can bring them with you to take after the test is done.
How long is the test?
The test takes about 4 hours, and includes registration, placing an IV, doing the test, and discharge.
Procedure:
The test is done lying down in a recliner. An endocrine nurse remains with you during the test.
After your blood pressure is checked and is in a safe range to continue with the test, an IV is placed in a vein in your arm or hand. After the IV is placed, the needle is removed and a small, flexible catheter remains. An IV is used so you don’t have to get multiple needle sticks.
After 30 minutes of lying flat, the endocrine nurse will get a blood sample and then you take the Clonidine by mouth.
Clonidine can cause your blood pressure to lower; therefore, your blood pressure is checked regularly during the test. Let the endocrine nurse know if you feel lightheaded or dizzy.
???????
Three hours after taking the Clonidine, another blood sample is drawn. The IV is removed and you are free to go home.
It is advisable that someone drive you home after the test because the Clonidine is still in your system and may be associated with some dizziness.
Possible side-effects:- Low blood pressure
- Lightheadedness/dizziness
- Dry mouth
- Drowsiness
- Other side-effects are related to the IV and include:
- Bleeding from the IV insertion site
- Bruising
- Lightheadedness
- Infection- rare as sterile technique is used
- Hematoma-blood under the skin
- Multiple punctures to locate veins
Results:
Results are available in a week. Please contact your doctor if you are not called about the result. -
Why is it done?
This test is used to differentiate between the various causes of elevated cortisol levels.
Cortisol is made in the adrenal glands which are above the kidneys.
???????Cortisol is important for regulating many body functions such as:- Response to stress
- Ability to fight infection
- Maintenance of blood pressure
- Regulation of blood sugar
Preparation:
The endocrine nurse will review your medicines, vitamins, and supplements with you. Some can affect your test results and may need to be stopped.
How long is the test?
The test takes approximately 2 ½-3 hours, and includes registration and triage, placing the IV, doing the test, and discharge.
Procedure:
This test requires specific time points, so planning is important.
Start dexamethasone tablets at 12 noon on day one. Take one tablet of dexamethasone every 6 hours for a total of 8 doses. The last dose will be at 6am on day 3.
Example-if your test is on Wednesday morning, you should start the pill on Monday at noon and continue every 6 hours through the rest of Monday and Tuesday. Take the last pill at 6 am on Wednesday.
Please do not take your medicines the morning you come to the Adrenal Center unless you have discussed this in advance with your physician performing the test. Patients are generally advised to hold their morning medications, but bring them with you to take after the test is done.
Blood is drawn 2 hours after your last dexamethasone pill; therefore, you must be at the Adrenal Center at 7 am so the IV can be placed at least 30 min before the 8 AM blood sample.
After the IV is placed, the needle is removed, and a small, flexible catheter remains. An IV is used, to avoid multiple needle sticks.
A manmade form of Corticotropin releasing hormone (CRH) is then given through your IV. CRH causes the pituitary gland in your brain to release adrenocorticotropic hormone (ACTH). ACTH then messages the adrenal gland to secrete cortisol.
Blood is drawn every 15 minutes for an hour.
The IV is removed and you are free to go home.
Possible side-effects:
Flushing may occur very briefly after the infusion of CRH is given. Hypotension has been described rarely if the infusion of CRH is given too quickly. This is unlikely as the protocol involves giving the medicine over 1-2 minutes.
Other side-effects are related to the IV and include:- Bleeding from the IV insertion site
- Bruising
- Lightheadedness
- Infection- rare as sterile technique is used
- Hematoma-blood under the skin
- Multiple punctures to locate veins
Results are available in a week. Please contact your doctor if you are not called about the result. -
Why is it done?
The Insulin Tolerance Test is done to evaluate patients who are suspected of having adrenal or growth hormone (GH) deficiencies. Adrenal insufficiency is a disorder in which the adrenal glands don't produce enough hormone called cortisol, which has an important function in the regulation of blood glucose, blood pressure, and overall wellbeing. A decrease in adrenal function may be related to a problem with the adrenal glands or a disorder affecting the pituitary gland, which is a small pea size gland below the brain. Growth hormone deficiency is usually caused by a disease affecting the pituitary gland. Patients with GH deficiency may have increased body fat, decreased muscle mass, low bone density, and reduced quality of life.
Precaution:
The test is not done in those above 65 years old, or those with heart diseases, seizures, or stroke.
Preparation:
The endocrine nurse will review all your medicines, vitamins, and supplements with you. Some drugs can affect the test and need to be stopped prior to the test. Patients who have been on GH therapy, need to be off GH for at least 30 days before the test. Patients taking hydrocortisone or prednisone for adrenal insufficiency need to hold their medications for 24 hours before the test (last dose in the morning the day before the test). The test needs to be done fasting in the morning. You should not take any food or drinks except water after midnight.
How long is the test?
The test takes about 3 hours. This includes registration, placing an IV, testing, and discharge.
Procedure:
The test is done lying down in a recliner. An endocrine nurse remains with you during the testing. After lying flat an IV is placed in a vein in your arm or hand. After the IV is placed, the needle is removed, and a small, flexible catheter remains. An IV is used, so you don’t have to get multiple needle sticks.
After the initial blood draw, the endocrine nurse will give you an injection of insulin through your IV to lower your blood glucose level. Following the injection of insulin, blood samples will be drawn at 15, 30, 45 and 60 minutes.
In about 10-20% of patients, a second dose of insulin may be necessary. At the end of the procedure, the nurse will give you a light snack with juice, making sure your blood glucose level is back to normal. During the test, patients experience symptoms of hypoglycemia (low blood glucose level). In healthy subjects, hypoglycemia results in an elevation of cortisol and GH levels. Patients with adrenal insufficiency and GH deficiency cannot raise their cortisol and GH levels, respectively.
Possible side-effects:
When your blood glucose drops, you will have one or more symptoms of hypoglycemia including sweating, rapid heart rate, headache, shakiness, and lightheadedness. The endocrine nurse will closely monitor you during the test. An intravenous injection of glucose will be given to you to rapidly increase your blood glucose level in the event of any severe symptoms.
Other side-effects are related to the IV and include:- Bleeding from IV insertion site
- Bruising
- Infection- rare as the sterile technique is used
- Hematoma-blood under the skin
- Multiple punctures to locate veins
Results are available in a week. Please contact your doctor if you are not called about the result. -
Why is it done?
The Resting Metanephrine and Catecholamine test is performed to see if there is a rare adrenal tumor (called a pheochromocytoma) or an extra adrenal tumor (called a paraganglioma). Both conditions can be associated with a number of symptoms including significant elevation in blood pressure, headache, excess sweating, chest pain and rapid heartbeat.
The test is performed fasting in the morning.
Preparation:
The endocrine nurse will review all your medicines, vitamins, and supplements with you. We ask that you do not take your morning medicines unless you have discussed this in advance with your physician performing the test.
You must fast after midnight. Water is permitted.
Do not exercise or smoke the morning of the test.
How long is the test?
Your visit is about 60 minutes, and includes registration, placing an IV, doing the test, and discharge.
Procedure:
The test is done with you lying flat (or as flat as possible). An IV is placed in a vein in your arm or hand. After the IV is placed, the needle is removed and a small, flexible catheter remains.
The lights are dimmed and after 30 minutes of lying flat, the endocrine nurse will get a blood sample. The test is done in our center as most outside labs cannot perform this specific protocol. The IV is removed and you are free to go home.
Possible side-effects:
The side-effects are related to the IV and include:- Bleeding from the IV insertion site
- Bruising
- Lightheadedness
- Infection- rare as sterile technique is used
- Hematoma-blood under the skin
- Multiple punctures to locate veins
Results are available in a week. Please contact your doctor if you are not called about the result. -
Why is it done?
The Saline Suppression test is done to diagnose primary aldosteronism or hyperaldosteronism, a condition in which the body makes too much of the hormone, aldosterone. It leads to high blood pressure and may be associated with low potassium levels in some patients.
The test involves drawing blood before and after you receive an infusion of saline (salt water). In patients without hyperaldosteronism, the infusion of saline causes the aldosterone level to lower. In patients with primary hyperaldosteronism, the aldosterone level does not lower to the same level as in patients without the disease.
Preparation:
The endocrine nurse will review all your medicines, vitamins, and supplements with you. Some medicines for blood pressure, your heart, and water pills (diuretics) can affect the test and may need to be stopped 2-4 weeks before the test.
You need to have your blood checked for a potassium level one week before the test. If your potassium is low, potassium pills will be given. Another blood draw may be needed to make sure the level is normal.
We ask that you eat a light snack if you need to take any medications with food. Otherwise, come to the clinic fasting. You may drink water as needed.
How long is the test?
The test takes about 5 hours. This includes registration, placing an IV, testing, and discharge. Feel free to bring music or something to read. Internet access is available.
Procedure:
The test is done sitting up in a chair. An endocrine nurse will check on you during the testing. An IV is placed in a vein in your arm or hand. After the IV is placed, the needle is removed, and a small, flexible catheter remains. An IV is used, so you don’t have to get multiple needle sticks.
A blood sample is drawn, and then you will get an infusion of saline (light salt water) over four hours through the IV. Another blood sample is done at the end of the infusion. Every hour, the endocrine nurse will check your blood pressure and heart rate, may listen to your heart and lungs, and check for swelling. This is done to make sure there are no effects from getting the saltwater.
The IV is removed, and you are free to go home.
Possible side-effects:
In some people, the salt water can cause:- Your blood pressure to rise
- A fast heart beat
- Feel short of breath
- Legs to swell
Other side-effects are related to the IV and include:- Bleeding from the IV insertion site
- Bruising
- Lightheadedness
- Infection- rare as a sterile technique is used
- Hematoma-blood under the skin
- Multiple punctures to locate veins
Results are available in a week. Please contact your doctor if you are not called about the result.
Meet the Experts
Co-Directors
Endocrinology
-
Adrian Sandra Dobs, M.D., M.H.S.

- Director, Johns Hopkins Clinical Research Network
- Professor of Medicine
- Professor of Oncology
-
Amir Hekmat Hamrahian, M.D.
- Medical Director of the Comprehensive Adrenal Center
- Associate Professor of Medicine
-
Roberto Salvatori, M.D.

- Medical Director, Johns Hopkins Pituitary Center
- Professor of Medicine
- Professor of Neurosurgery
-
Prasanna Santhanam, M.B.B.S., M.D.

- Associate Director , Communications, Division of Endocrinology
- Associate Professor of Medicine
- Associate Professor of Oncology
Surgeons
-
Aarti Mathur, M.D., Ph.D.

- Associate Vice Chair of Faculty Development
- Associate Professor of Surgery
- Associate Professor of Oncology
-
Lilah Fran Morris-Wiseman, M.D.

- Chief, Johns Hopkins Division of Endocrine Surgery
- Associate Professor of Surgery
- Associate Professor of Oncology
-
Nirmish Singla, M.D., M.Sc.

- Director of Translational Research in GU Oncology
- Director, Kidney Cancer Program
- Co-Director, Upper Tract Urothelial Cancer (UTUC) Program
- Vice Chair and Physician Advisor for Quality, Safety, & Service, Brady Urological Institute
- Associate Professor of Urology
- Associate Professor of Oncology
Medical Oncology
Gynecology and Obstetrics
-
Torre Leigh Halscott, M.D., M.S.

- Medical Director of Nelson 2 Clinic
- Assistant Professor of Gynecology and Obstetrics
-
Jason Vaught, M.D.

- Director, Labor and Delivery
- Director, Advanced Obstetric Surgery Center
- Robert E. Meyerhoff Professor
- Associate Professor of Gynecology and Obstetrics
- Associate Professor of Surgery
Diagnostic and Inverventional Radiology
-
Elliot K Fishman, M.D.

- Elliot K. Fishman Professorship in Radiology
- Professor of Radiology and Radiological Science
- Professor of Oncology
- Professor of Surgery
- Professor of Urology
-
Brian Philip Holly, M.D.
- Program Director, Interventional Radiology Integrated Residency
- Assistant Professor of Radiology and Radiological Science
Radiation Oncology
-
Jeffrey Meyer, M.D., M.S.
- Associate Professor of Radiation Oncology and Molecular Radiation Sciences
- Associate Professor of Oncology
- Associate Professor of Surgery
-
Amol Kumar Narang, M.D.
- Assistant Professor of Radiation Oncology and Molecular Radiation Sciences
- Assistant Professor of Oncology
- Assistant Professor of Surgery
Pathology
-
Andres Matoso, M.D.

- Acting Director of the Genitourinary Fellowship Program
- Associate Professor of Pathology
- Associate Professor of Oncology
- Associate Professor of Urology
Genetics
Katie Fiallos, M.D.

Dana Petry, M.D.