Lasker Award Winner Gregg Semenza, M.D., Ph.D.
C. Michael Armstrong Professor of Genetic Medicine, Pediatrics, Medicine, Oncology, Radiation Oncology, and Biological Chemistry
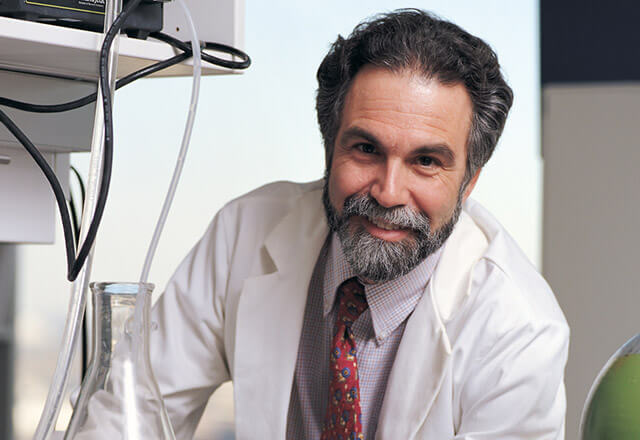 Dr. Gregg Semenza
Dr. Gregg SemenzaGregg L. Semenza, M.D., Ph.D. of the Johns Hopkins University School of Medicine was awarded the 2016 Albert Lasker Basic Medical Research Award by the Albert and Mary Lasker Foundation. Semenza, along with co-award winners William G. Kaelin, Jr., M.D. of the Dana-Farber Cancer Institute and Peter J. Ratcliffe of Oxford University, were recognized for their “discovery of essential pathways by which human and animal cells sense and adapt to the presence of oxygen.”
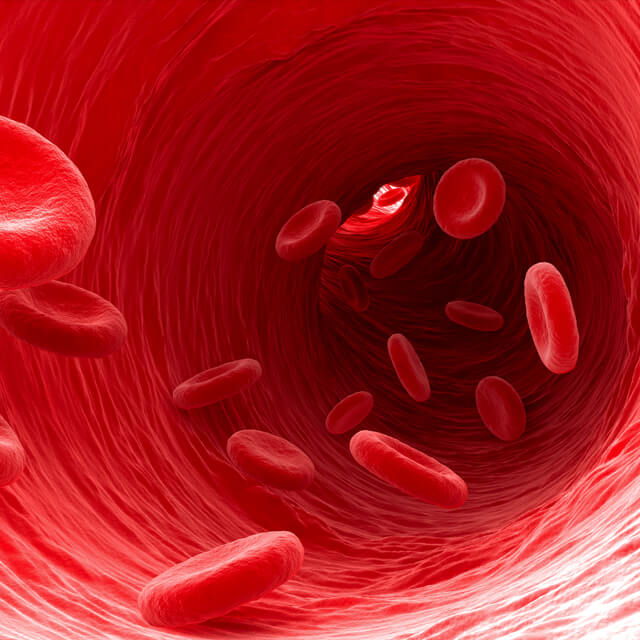
In 1992, Semenza and co-authors announced their ground-breaking discovery of hypoxia inducible factor 1 or HIF-1, which helps cells cope with low oxygen levels. The discovery has far-reaching implications in for understanding low oxygen health conditions like coronary artery disease and tumor growth. Since then Semenza has identified genes turned on by HIF-1 that control energy production, the making of red blood cells and the growth of blood vessels. He currently is studying the role of HIF-1 in cancer, ischemia and chronic lung disease, the most common causes of mortality in the U.S. population.
Implications for Cancer
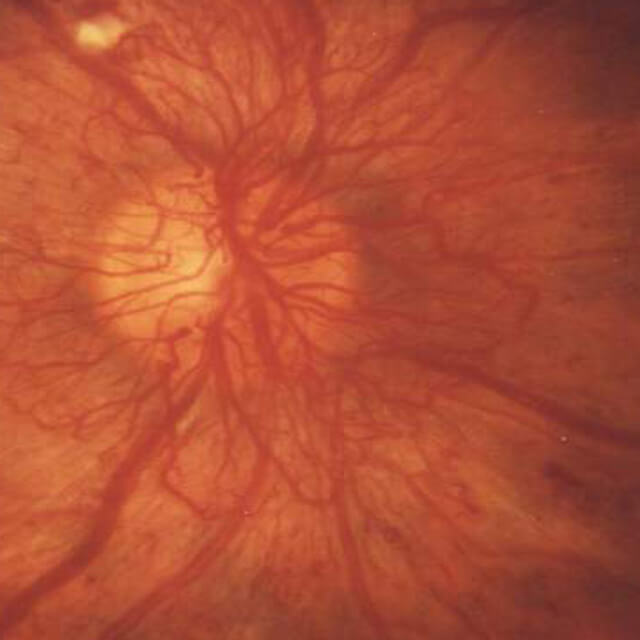
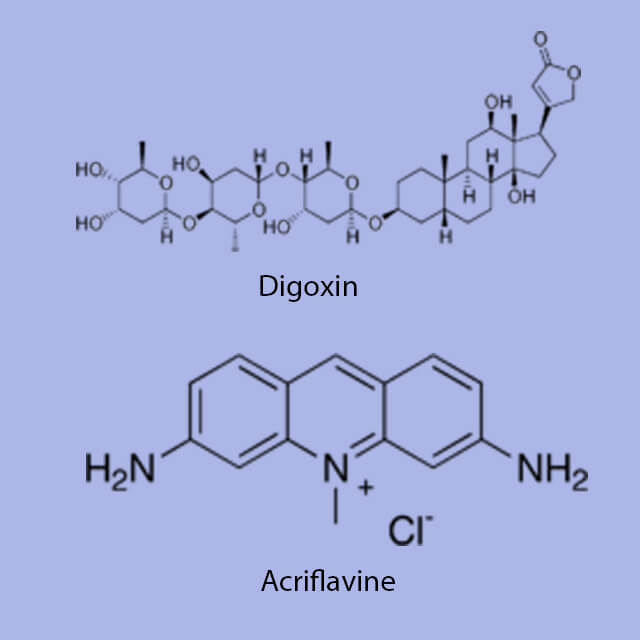
Tumors face a central problem: as they grow larger, cells near the middle are increasingly cut off from the body’s oxygen supply. Since HIF senses oxygen levels, it’s critical to stimulating the growth of new vessels to supply the tumor. Semenza and others are working to find and test therapeutics that would block HIF, which may prove a fatal chink in the armor of some tumors.
Implications for Diabetes
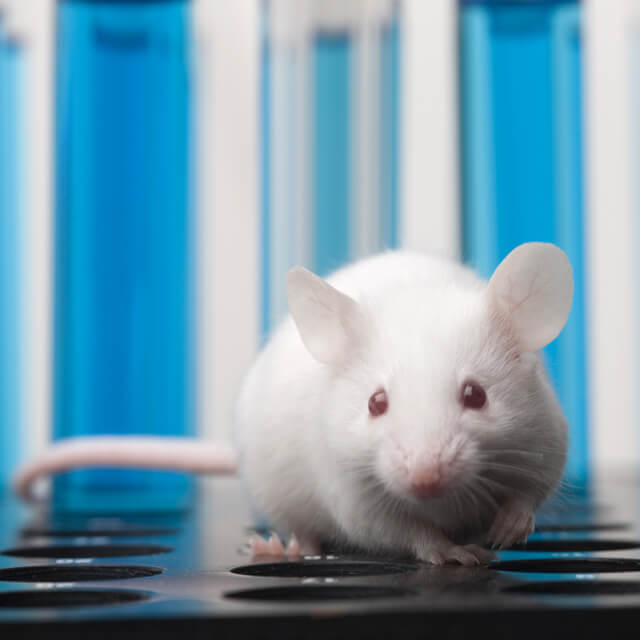
Relative to people without the disease, patients with type 2 diabetes face a high risk of losing a limb to amputation due to poor circulation. Semenza’s work suggests HIF-1 could be the key to restoring circulation before it’s too late. By treating diabetic mice with a virus engineered to increase HIF-1 production, his team was able to increase blood flow to their limbs.
What's Next?
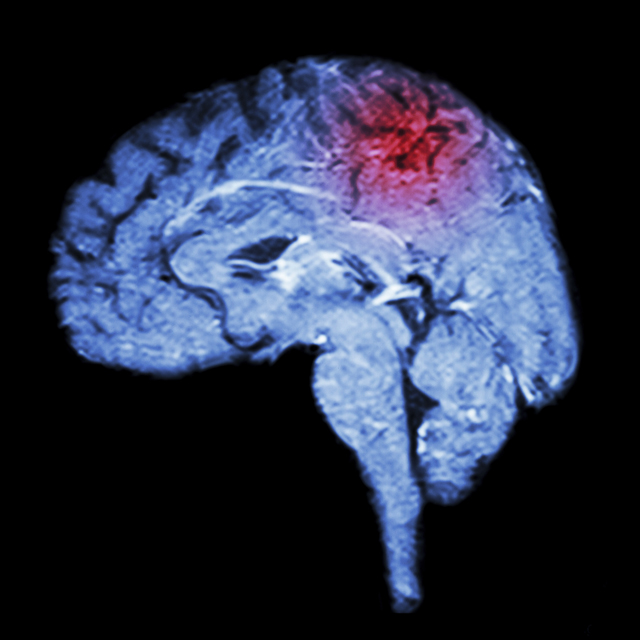
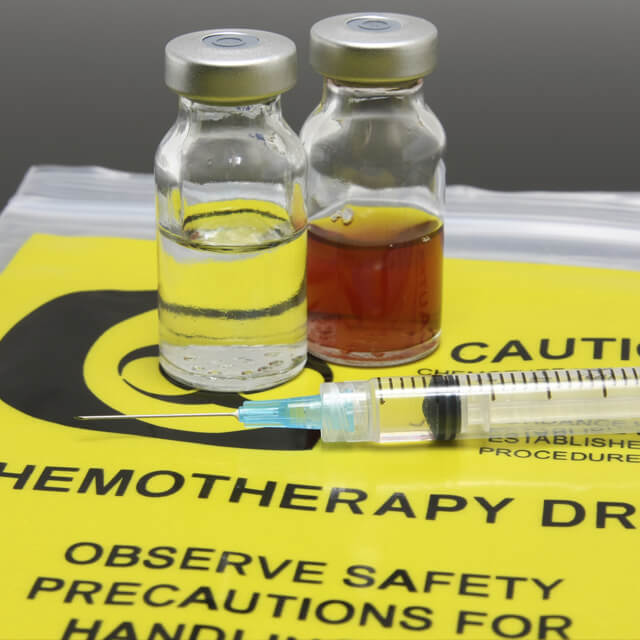
Researchers are at work on potential therapies that would change HIF-1 activity to treat conditions such as cancer, diabetes and stroke. For example, a drug known as GSK1278863 is being clinically tested as a treatment for patients with anemia associated with chronic kidney disease. The drug represses HIF to maintain hemoglobin levels.
Dr. Semenza on the Discovery of HIF-1
Gregg Semenza, M.D., Ph.D. talks about his seminal discovery of the protein HIF-1 in the 1990s, its potential applications to treating anemia and cancer, and life as a researcher.
The Joy of Scientific Discovery
Gregg Semenza, M.D., Ph.D., of the Johns Hopkins McKusick-Nathans Institute of Genetic Medicine on the excitement and unpredictability of being a scientist.

#TomorrowsDiscoveries: Chemotherapy-Resistant Breast Cancer Stem Cells
While chemotherapy attacks and kills 99 percent of breast cancer cells, it leaves behind chemotherapy-resistant cancer stem cells, which can later cause metastatic tumors. Dr. Gregg Semenza’s team has identified a way to overcome the resistance of cancer stem cells to chemotherapy, completely eradicating breast tumors in mice.

-
Gregg Semenza Lab
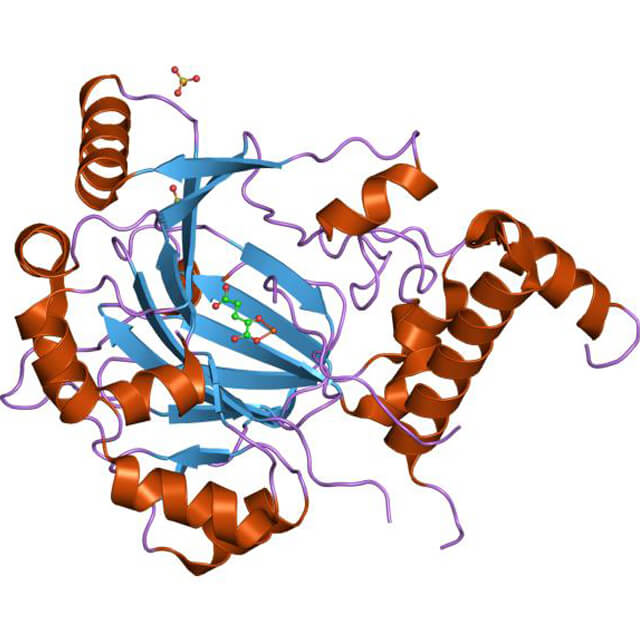
The Gregg Semenza Lab studies the molecular mechanisms of oxygen homeostasis. We have cloned and characterized hypoxia-inducible factor 1 (HIF-1), a basic helix-loop-helix transcription factor.
Current research investigates the role of HIF-1 in the pathophysiology of cancer, cerebral and myocardial ischemia, and chronic lung disease, which are the most common causes of mortality in the U.S.